【概 要】
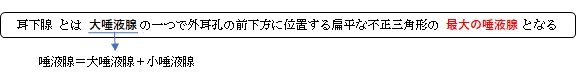
耳下腺は顎下腺に次いで唾液の分泌量が多く
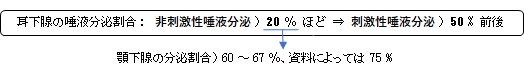
非刺激性唾液分泌 : 外部からの刺激(例:食べ物を見たり噛んだり)が無い状態で自然と分泌される唾液
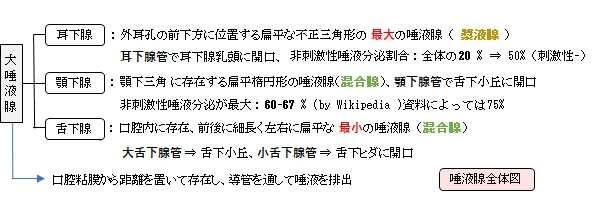
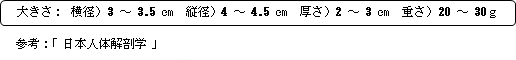
以下は「日本人体解剖学」の解説文となる。
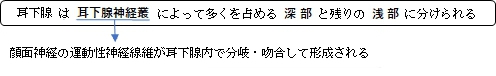
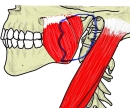
耳介の前方にある大部を浅部(顔面神経の上にある)といい、耳下腺咬筋部に位置する。残りの小部を深部(顔面神経の下にある)といい、下顎後窩に位置する。
下顎後突起:耳下腺の後部のことで、下顎後窩に深く入り、その末端は顎関節の後下側に接している。
■面・縁■
外面:わずかに膨隆し強靭な耳下腺筋膜に覆われる。
内面:咬筋に接し、内頚動・静脈(又は下顎高静脈?)が見られる。
下縁:胸鎖乳突筋の前縁に接する。
上縁:頬骨弓および外耳道に接する。
|

|

|
|
大唾液腺-1 |
大唾液腺-2 |
耳下腺・咬筋 |
耳下腺(横断面) |
|
|
|
|
耳下腺・神経叢 |
耳下腺神経叢からの枝 |
耳下腺と筋 |
|
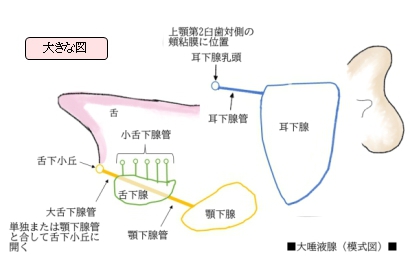
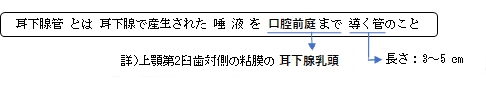
【耳下腺管】
副耳下腺:耳下腺管沿いにしばしば出現する大きさ・形状不定の唾液腺でその導管は耳下腺管に合する。
■走 行■
1. 耳下腺の前上部より出る。
2. 頬骨弓の下約1㎝のところを咬筋の外側面に沿って前走する。
3. 頬脂肪体縁に至ってからほぼ直角に内側方に曲がる。
4. 頬筋および頬粘膜を貫通し、耳下腺乳頭(上顎第2臼歯対側の頬粘膜に存在)に開口する。
【脈管/神経】
以下が耳下腺に分布する脈管および神経となる。 参考:日本人体解剖学
動 脈:浅側頭動脈および顎動脈の枝
静 脈 : 耳下腺静脈は下顎後静脈に、耳下腺枝は顔面静脈にそそぐ。
リンパ管 : 浅・深耳下腺リンパ節および浅・深頚リンパ節に入る。
神 経 :
交感神経線維)頚部交感神経から、外頚動脈周囲の交感神経叢を経て耳下腺に入る。
副交感神経線維(舌咽神経の分泌線維))は小錐体神経として耳神経節に入り、ついで
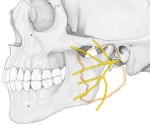
耳介側頭神経となり、耳下腺枝を耳下腺に送る。顔面神経の末梢枝は耳下腺の内部で
複雑な神経叢をつくる。
【Wikipedia】
以下は「Wikipedia」の解説文となる。
The parotid gland is a major salivary gland in many animals. In humans, the two parotid glands are present on either side of the mouth and in front of both ears. They are the largest of the salivary glands. Each parotid is wrapped around the mandibular ramus, and secretes serous saliva through the parotid duct into the mouth, to facilitate mastication and swallowing and to begin the digestion of starches. There are also two other types of salivary glands; they are submandibular and sublingual glands.
The word parotid (paraotic) literally means "beside the ear".
Structure
The parotid glands are a pair of mainly serous salivary glands located below and in front of each ear canal, draining their secretions into the vestibule of the mouth through the parotid duct.[2] Each gland lies behind the mandibular ramus and in front of the mastoid process of the temporal bone. The gland can be felt on either side, by feeling in front of each ear, along the cheek, and below the angle of the mandible.[3]
The parotid duct, a long excretory duct, emerges from the front of each gland, superficial to the masseter muscle. The duct pierces the buccinator muscle, then opens into the mouth on the inner surface of the cheek, usually opposite the maxillary second molar. The parotid papilla is a small elevation of tissue that marks the opening of the parotid duct on the inner surface of the cheek.[3]
The gland has four surfaces — superficial or lateral, superior, anteromedial, and posteromedial. The gland has three borders — anterior, medial, and posterior. The parotid gland has two ends — superior end in the form of small superior surface and an inferior end (apex).
A number of different structures pass through the gland. From lateral to medial, these are:
Location
- Superficial or lateral relations: The gland is situated deep to the skin, superficial fascia, superficial lamina of investing layer of deep cervical fascia and great auricular nerve (anterior ramus of C2 and C3).
- Anteromedial relations: The gland is situated posterolaterally to the mandibular ramus, masseter and medial pterygoid muscles. A part of the gland may extend between the ramus and medial pterygoid, as the pterygoid process. Branches of facial nerve and parotid duct emerge through this surface.
- Posteromedial relations: The gland is situated anterolaterally to mastoid process of temporal bone with its attached sternocleidomastoid and digastric muscles, styloid process of temporal bone with its three attached muscles (stylohyoid, stylopharyngeus, and styloglossus) and carotid sheath with its contained neurovasculature (internal carotid artery, internal jugular vein, and 9th, 10th, 11th, and 12th cranial nerves).
- Medial relations: The parotid gland comes into contact with the superior pharyngyeal constrictor muscle at the medial border, where the anteromedial and posteromedial surfaces meet. Hence, a need exists to examine the fauces in parotitis.
Blood supply
The external carotid artery and its terminal branches within the gland, namely, the superficial temporal and the Maxillary artery, supply the parotid gland. Venous return is to the retromandibular veins.
Lymphatic drainage
The gland is mainly drained into the preauricular or parotid lymph nodes which ultimately drain to the deep cervical chain.
Nerve supply
The parotid gland receives both sensory and autonomic innervation. General Sensory innervation to the parotid gland, its sheath, and the overlying skin is provided by the great auricular nerve. The autonomic innervation controls the rate of saliva production and is supplied by the glossopharyngeal nerve.[4] Postganglionic sympathetic fibers from superior cervical sympathetic ganglion reach the gland as periarterial nerve plexuses around the middle meningeal artery and their function is mainly vasoconstriction. The cell bodies of the preganglionic sympathetics usually lie in the lateral horns of upper thoracic spinal segments. Preganglionic parasympathetic fibers leave the brain stem from inferior salivatory nucleus in the glossopharyngeal nerve and then through its tympanic and then the lesser petrosal branch pass into the otic ganglion. There, they synapse with postganglionic fibers which reach the gland by hitch-hiking via the auriculotemporal nerve, a branch of the mandibular nerve.
【語句】
・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・:
【イラストを掲載しているサイト】
・ イラストや写真を掲載しているサイト-Ⅰ
・ イラストや写真を掲載しているサイト-Ⅱ
・ イラストや写真を掲載しているサイト-Ⅲ
・ イラストや写真を掲載しているサイト-Ⅳ
・ イラストや写真を掲載しているサイト-Ⅴ