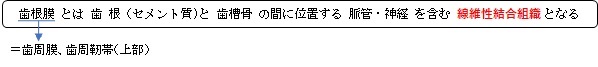
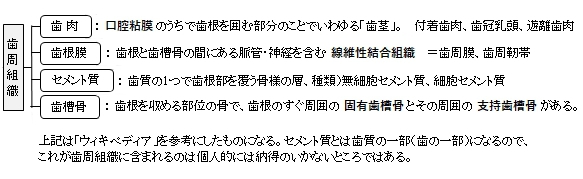
歯根膜は歯周組織の1つとなる
【シャーピー線維の走行方向】(参考:日本人体解剖学)
起始 : シャーピー線維の線維束はセメント質内から起こる。
歯根上部 : 上方へ、特に歯肉の乳頭に向って放散し、次いで水平方向へ
歯根中部~下部 : 上方に向かう。
根端部 : 下方に向かう。
以下は「日本人体解剖学」の解説文となる。
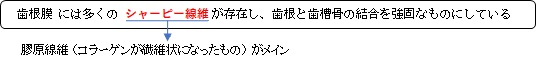
「(歯根膜は)歯槽の骨と歯根との間をうめる線維性結合組織である。弾性繊維に乏しく、
膠原線維束からなるシャーピー線維に富み、また多数の神経線維に貫通される。歯槽入
口部では、歯頚および歯槽縁を連ねる強靭な歯輪状靭帯(歯周靭帯)となる。
シャーピー線維は、歯の植立を堅固にするのに役立つ。線維束はセメント質内から起こる。
歯根の上部では上方、とくに歯肉の乳頭に向かって放散し、それにつぐ部では水平に走り
歯槽骨内に入る。中間部から下部では逆に上方に向かい、骨端部では下方に向かって走り、
力学的に咬合圧による弾性体として作用する。 」
以下は「Wikipedia」の「periodontal ligament」の解説文となる。
The periodontal ligament, commonly abbreviated as the PDL, is a group of specialized connective tissue
fibers that essentially attach a tooth to the alveolar bone within which it sits. It inserts into root cementum
one side and onto alveolar bone on the other.
The PDL consists of principal fibres, loose connective tissue, blast and clast cells, oxytalan fibres and Cell
Rest of Malassez.[2]
The main principal fiber group is the alveolodental ligament, which consists of five fiber subgroups: alveolar
crest, horizontal, oblique, apical, and interradicular on multirooted teeth. Principal fibers other than the
alveolodental ligament are the transseptal fibers.
All these fibers help the tooth withstand the naturally substantial compressive forces that occur during
chewing and remain embedded in the bone. The ends of the principal fibers that are within either cementum
or alveolar bone proper are considered Sharpey fibers.
- Alveolar crest fibers (I) run from the cervical part of the root to the alveolar bone crest
- Horizontal fibers (J) attach to the cementum apical to the alveolar crest fibers and run perpendicularly
- from the root of the tooth to the alveolar bone..
- Oblique fibers (K) are the most numerous fibers in the periodontal ligament, running from cementum in
- an oblique direction to insert into bone coronally. These fibres resist vertical & intrusive forces
- Apical fibers are found radiating from cementum around the apex of the root to the bone, forming base
- of the socket or alveolus.
- Interradicular fibers are only found between the roots of multirooted teeth, such as premolars and molars.
- They extend from radicular cementum to interradicular alveolar bone.
【Transseptal fibers】
Transseptal fibers (H) extend interproximally over the alveolar bone crest and are embedded in the cementum
of adjacent teeth; they form an interdental ligament. These fibers keep all the teeth aligned. These fibers may
be considered as belonging to the gingival tissue because they do not have an osseous attachment.[3]
【Loose connective tissue】
Loose connective tissue contains fibres, extracellular matrix, cells, nerves and blood vessels. The extracellular
compartment consists of Type 1, 3, and 5 collagen fibers bundles embedded in intercellular substance. The PDL
collagen fibers are categorized according to their orientation and location along the tooth. The cells include
fibroblast, defence cells and undifferentiated mesenchymal cells.
【Cell Rest of Malassez】
These groups of epithelial cells become located in the mature PDL after the disintegration of Hertwig epithelial
root sheath during the formation of the root.[2]They form a plexus that surrounds the tooth. Cell Rests of
Malassez might proliferate during inflammation which may lead to radicular cyst formation in later life.
【Oxytalan fibres】
Oxytalan fibres are unique to the PDL and are elastic in nature. It inserts into cementum and runs in 2 directions;
parallel to root surface and oblique to root surface. The function is thought to maintain the patency of blood
vessels during occlusal loading. Further research is needed to determine the function of oxytalan fibres.[4]
The PDL substance has been estimated to be 70% water, which is thought to have a significant effect on the
tooth's ability to withstand stress loads. The completeness and vitality of the PDL are essential for the
functioning of the tooth.
The PDL ranges in width from 0.15 to 0.38mm with its thinnest part located in the middle third of the root.[5]
The width progressively decreases with age.
The PDL is a part of the periodontium that provides for the attachment of the teeth to the surrounding alveolar
bone by way of the cementum.
The PDL appears as the periodontal space of 0.4 to 1.5 mm[citation needed] on radiographs, a radiolucent area
between the radiopaque lamina dura of the alveolar bone proper and the radiopaque cementum.
PDL cells are one of the many cells derived from the dental follicle and this occurs after crown formation is
completed and when the roots start developing. These cells will remodel the dental follicle to form the PDL.[5]
Formation of PDL will start at the cementoenamel junction and proceeds in an apical direction.[6]
Effects of Mechanical Forces on the Development of PDL[edit]
Movement of teeth is determined by two factors; deposition of bone on the tension side and resorption of the
bone on the compression side of the periodontal ligament (PDL). During this movement, bone remodelling is
initiated by the PDL in which forces are transmitted from the tooth to the alveolar bone. Fibroblasts of the
PDL will react to mechanical stress, therefore affecting osteoblastogenesis and osteoclastogensis of the cells.
When mechanical stimuli are introduced to the cells osteocytes in the PDL will differentiate into osteoclasts
which will then reform and remodel the bone structure in the affected area. For example, orthodontic treatment
involves application of a mechanical force on to the teeth to align them and this is done through this complex
combination of physical and cellular processes.[7]
Functions of PDL are supportive, sensory, nutritive, and remodelling.[8]
Support
The PDL is a part of the periodontium that provides for the attachment of the teeth to the surrounding alveolar
bone by way of the cementum. PDL fibres also provide a role in load transfer between the teeth and alveolar bone.
(PDL fibres absorb and transmit forces between teeth and alveolar bone. It acts as an effective support during
the masticatory function.)[9]
Sensory
PDL is heavily innervated; it involves mechanoreception, nociception and reflexes. Periodontal mechanoreceptors
are present in pdl. They will transmit information about the stimulated tooth, direction and amplitude of forces.[10]
Nutritive
It maintains the vitality of the surrounding cells. (PDL is heavily anastomosed). There are 3 principal sources of
blood vessels which are apical vessels, perforating vessels and gingival vessels. Apical vessels originate from vessels
that supply the pulp. Perforating vessels originate from lamina dura and the vessels perforate the socket wall
(cribriform plate). Gingival vessels are derived from the gingival tissue. Outer layers of blood supply in PDL may
help in mechanical suspension and support of the tooth while inner layers of blood vessels supply surrounding
PDL tissues.[11]
Remodeling
There are progenitor cells in the periodontal ligament that can differentiate into osteoblasts for the physiological
maintenance of alveolar bone and, most likely, for its repair as well.
【 語 句 】
・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・: ・:
・: ・: ・: ・: ・: ・:
■ 写真やイラストを掲載しているサイト ■
・イラストを掲載しているサイト-Ⅰ
・イラストを掲載しているサイト-Ⅱ
・イラストを掲載しているサイト-Ⅲ
・イラストを掲載しているサイト-Ⅳ